DOD CDMRP Translational Team Award: CA150590
PI: L.B. Schook
Partnering PIs: R.C. Gaba, University of Illinois at Chicago
F.E. Boas, Memorial Sloan Kettering Cancer Center
K.T. Brown, Memorial Sloan Kettering Cancer Center
S.B. Solomon, Memorial Sloan Kettering Cancer Center
Award Dates: August 1, 2016 - July 30, 2019
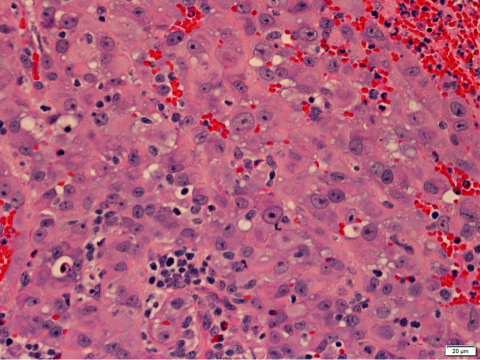
This grant addresses the Peer Reviewed Cancer Research Program Topic Area of hepatocellular carcinoma (HCC), which is the fifth most common cancer globally and the third most common cause of cancer-related death worldwide, accounting for more than 600,000 deaths each year. Effective treatments for HCC are limited and only available to few patients. Many factors, including underlying liver disease, tumor size or location prevent surgery from being a viable therapeutic option. Thus, 85% of HCC patients require other therapeutic options, namely interventional radiology (IR) locoregional therapies (LRTs), defined as minimally invasive, image-guided therapies. Our proposal aims to address gaps in detection, diagnosis, and treatment of liver cancer, particularly for the military and Veteran populations and their families, who are at increased risk. Many clinical trials have been conducted to investigate optimal management of HCC; however, several important questions remain, further demonstrating the critical need for a relevant large animal model. The Oncopig cancer model (OCM) was created to provide a relevant, biologically analogous HCC model, and it offers an efficient, faster, and less expensive testing of promising HCC therapies. Our hypothesis is that genetic alteration of pathways, commonly disrupted in human cancers, will provide a standardized disease-site porcine tumor model, analogous to human tumors, and support therapeutic interventions. Thus, we aim to: (1) induce and characterize multifocal HCC in the OCM; (2) induce cirrhosis in the tumor host environment; (3) validate OCM for translation to human clinical trials; and (4) test the feasibility of hepatic artery embolization in OCM.
Study Design: The Oncopig currently provides a model system for inducing orthogonal adenocarcinoma using catheters by IR, active surveillance of tumor detection and growth consisting of laboratory and imaging assessments. Oncopig surveillance will be measured using adapted human measures, including performance status and Child-Pugh score. Cancer will be induced in both lobes of the liver; however, only one lobe will be embolized, allowing each Oncopig to act as its own control. Cirrhosis induction provides a comorbidity environment for development prior to therapeutic interventions. Tumor angiographic appearance will be characterized according to multiple parameters, including hypervascularity and tumor neovasculature. Liver tumor embolization will be performed under direct fluoroscopic observation. Microsphere administration will continue until no further tumor vascular blush is identified and a substasis angiographic endpoint is attained.
Collaboration/Translational Aspects: The program harnesses the complementary expertise of each investigator, representing the University of Illinois Cancer Center (UICC) and Memorial Sloan Kettering Cancer Center (MSKCC). UICC expertise created the OCM model for cancer research and has partnered with clinician-scientists, as Partnering Principal Investigators (PIs) to validate and refine the model for critically important translation into human clinical trials. The PIs have worked effectively to establish a strong interactive research initiative, including the generation of the Oncopig HCC model that provides the foundation for this proposal. Partnering PIs Gaba and Boas are early-career investigators who both have substantial roles in the design and conduct of this project. Partnering PIs Gaba, Solomon, Brown, and Boas are practicing IRs who are directly responsible for the care of HCC patients. Their clinical expertise, paired with Schook's expertise in comparative genomics and animal modeling, represents the optimal team to validate and translate the novel OCM for study of human cancers. Co-investigators have met face-to-face at MSKCC and will continue to regularly meet virtually and face-to-face for exchange of ideas. Schook will produce Oncopigs for cancer induction and treatment at MSKCC and UIC, representing the most efficient use of available resources. Oncopigs will be dispersed to two clinical sites for epigenetic experimental control.Military Relevance and Impact: HCC is exceedingly common in the U.S. Veteran population due to a high incidence of alcoholic cirrhosis and viral hepatitis. The OCM is a novel experimental model in which these highly relevant comorbidities are induced for comprehensive investigation and translation to highly impactful and of great benefit to military and Veteran populations.
Innovation: Clinically, the Oncopig provides a highly relevant cancer model due its similarities in size, anatomy, physiology, genetics, and drug metabolism compared to humans and provides a platform for comparing and analyzing different liver directed therapies. Due to similarities in its anatomy, physiology, and metabolism, the Oncopig provides a model where comorbidities that are highly relevant to military and Veteran populations (cirrhosis, fibrosis, obesity) can be induced during tissue-targeted oncogenesis. The OCM permits IR-enabled delivery of tumor-inducing signals for site-specific primary and metastatic tumor induction. Furthermore, the Oncopig enables examination of explanted livers after embolization, which is not possible in human trials. The Oncopig, with this investigative team, represents a new paradigm to investigate HCC from a new perspective. Hence, this model and team have the potential to close gaps in screening, early detection, diagnosis, and treatment and to improve efficacy of therapeutic options.